ABSTRACT
-
Background
- The COVID-19 pandemic and the implementation of social distancing have been reported to negatively impact cardiovascular-related health behaviors. However, the effects of lifting social distancing restrictions on these health behaviors remain unclear. This study investigated public awareness and behavioral changes related to cardiovascular disease prevention after the end of social distancing.
-
Methods
- Between June 5 and June 12, 2023, 2,000 adults participated in the 2023 Cardiovascular Disease Prevention Awareness Survey in Korea. The survey comprehensively addressed sociodemographic factors, cardiometabolic disease history, cardiovascular disease concern, prevention awareness, and behavioral changes after the end of social distancing. Logistic regression analyses were performed to assess the associations between behavioral changes and sociodemographic factors.
-
Results
- Cardiovascular disease ranked as the second most feared disease (most feared, 18.0%; second most feared, 26.3%) after cancer (most feared, 42.3%; second most feared, 21.7%). Among nine cardiovascular disease prevention recommendations, stress management, being physically active, and maintaining a healthy diet were perceived as the most challenging recommendations. After the end of social distancing, there were more positive changes than negative changes in smoking, alcohol consumption, dietary habits, physical activity, and healthcare service use, whereas stress management more frequently changed negatively (40.0%) than it changed positively (19.5%).
-
Conclusions
- Positive changes in cardiovascular-related health behaviors, except for stress management, were observed after the end of social distancing. Further research is necessary to fully comprehend the impact of discontinuing social distancing practices.
-
Keywords: Cardiovascular diseases; Prevention and control; COVID-19; Physical distancing; Korea
INTRODUCTION
- Cardiovascular disease (CVD) constitutes a significant global public health challenge and contributes substantially to the worldwide burden of disease [1]. Despite a decrease in age-specific death rates for CVD, global deaths from CVD have been increasing rapidly [2,3]. This increase is largely due to the aging of the population [2–4]. In Korea, the proportion of the elderly population is rapidly increasing, reaching 18.4% in 2023 [5]. Thus, reducing the burden of CVD has become an increasingly important priority.
- CVD is preventable through health behaviors. The American Heart Association (AHA) recently introduced Life’s Essential 8, emphasizing four health behaviors (diet, physical activity, nicotine exposure, and sleep health) and four health factors (body mass index, blood lipids, blood glucose, and blood pressure) that are essential for CVD prevention [6]. Several studies have also underscored the importance of health behaviors in preventing CVD [7–10]. Likewise, the Korea Disease Control and Prevention Agency (KDCA) has promoted nine lifestyle recommendations for preventing and managing CVD [11].
- The COVID-19 pandemic and the subsequent implementation of social distancing have been reported to induce adverse changes in health behaviors. The restriction of outdoor activities and social interactions, a direct consequence of the pandemic, contributed to a notable decline in physical activity levels and a rise in depression [12,13]. Concurrently, in the United States, there was a discernible decrease in hospital admissions and medical procedures pertaining to myocardial infarction during the pandemic period [14]. Further emphasizing these shifts, the Korean Society of Cardiovascular Disease Prevention (KSCP) conducted a 2022 Cardiovascular Disease Prevention Awareness Survey. The survey results brought attention to the pandemic's detrimental effects on cardiovascular health, revealing negative changes in crucial health behaviors such as diet, exercise, and stress management [15].
- In Korea, social distancing ended in April 2022, but the specific changes in health behaviors following this policy shift are not well understood. Therefore, this study aimed to examine public awareness regarding CVD prevention and the subsequent changes in cardiovascular-related health behaviors after the end of social distancing. In addition, we explore demographic factors that may contribute to variation in the observed effects.
METHODS
- Ethics statement
- All participants of the 2023 Cardiovascular Disease Prevention Awareness Survey provided written informed consent before participating.
- Data source
- This study utilized data from the 2023 Cardiovascular Disease Prevention Awareness Survey. The survey was conducted in June 2023 by the KSCP to assess public awareness levels of CVD. A proportionate quota sampling method was used for participant selection. A total of 2,000 adults from 17 provinces in Korea completed a structured questionnaire online or via mobile devices, from June 5 to June 12, 2023.
- Questionnaires and variables
- The questionnaire comprised five elements: sociodemographic characteristics, history of cardiometabolic disease, CVD concern and self-assessed CVD likelihood, awareness and practice of CVD prevention, and changes in health behaviors after the end of social distancing.
- Sociodemographic characteristics included age, sex, marital status (single, married, bereaved/separated/divorced), monthly household income (<3 million, 3 to <6 million, ≥6 million KRW), and education (middle school or below, high school, college or above). Respondents reported their history of cardiometabolic diseases, including coronary heart disease, cerebrovascular disease, hypertension, diabetes, and dyslipidemia.
- CVD concern and self-assessed likelihood were measured in comparison with other diseases known to have high mortality or disability-adjusted life years based on the Korean Burden of Disease Study—specifically, cancer, musculoskeletal disorders, dementia, and psychiatric disorders [16]. Regarding CVD prevention, respondents were assessed for their awareness and practice of CVD prevention recommendations, utilizing the CVD prevention guideline from the KDCA [11]. This guideline includes nine recommendations: (1) do not smoke; (2) drink no more than one or two drinks per day; (3) eat a healthy diet such as unsalted and nutritionally balanced food; (4) engage in moderate exercise for at least 30 minutes every day; (5) keep an appropriate body weight and waist circumference; (6) reduce stress and improve mental health; (7) regularly check blood pressure, blood sugar, and cholesterol and manage them; (8) treat hypertension, diabetes, and dyslipidemia; and (9) be aware of the emergency symptoms of stroke and myocardial infarction, and go to the hospital immediately if symptoms occur. For these nine recommendations, respondents were asked to assess their importance for preventing CVD, and to choose the most, second and third most difficult item to practice.
- We examined changes in six health-related lifestyle habits following the end of social distancing, based on the KDCA's CVD prevention guideline: (1) smoking frequency and amount; (2) alcohol consumption frequency and amount; (3) adherence to a healthy diet; (4) frequency and amount of physical activity; (5) stress and mental health; and (6) healthcare service use and management of symptoms or diseases [11]. Responses were classified into three categories: negative change, no or minimal change, and positive change.
- Statistical analysis
- Descriptive analyses were performed to examine the distribution of respondents’ sociodemographic characteristics, CVD concern, CVD prevention awareness, and behavioral changes after the end of social distancing. Multivariate logistic regression analyses were performed to evaluate associations between behavioral changes after the end of social distancing and sociodemographic factors. Adjustments were made for all sociodemographic variables. All statistical analyses were conducted using SAS ver. 9.4 (SAS Institute Inc).
RESULTS
- Respondents' characteristics
-
Table 1 provides an overview of the survey respondents’ sociodemographic characteristics and history of cardiometabolic diseases. The age distribution was as follows: 21.4% of participants were in their 20s, 22.3% were in their 30s, 27.3% were in their 40s, and 29.1% were in their 50s or older. The proportion of male respondents was 51.4%. The prevalence of cardiometabolic disease history was as follows: 2.3% for coronary heart disease, 1.7% for cerebrovascular disease, 18.5% for hypertension, 7.5% for diabetes, and 21.1% for dyslipidemia.
- Concern and prevention of CVD
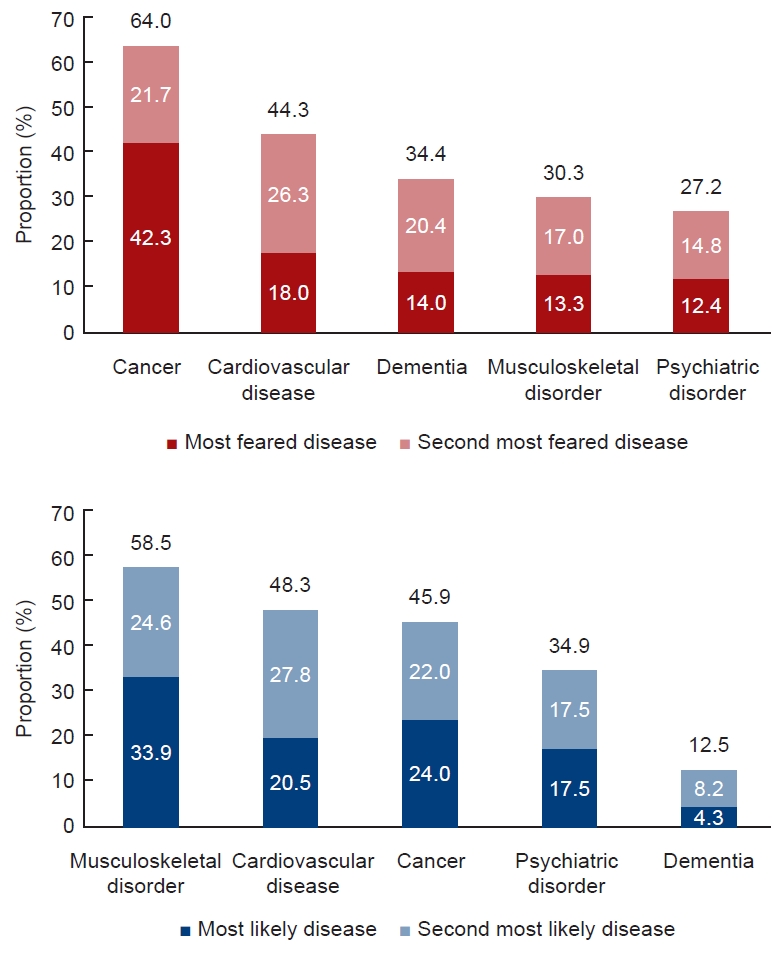
- Among the five diseases included in the survey, CVD ranked as the second most feared condition (most feared, 18.0%; second most feared, 26.3%) following cancer (most feared, 42.3%; second most feared, 21.7%) (Fig. 1A). CVD also ranked as the second most likely disease to occur within a decade (most likely, 20.5%; second most likely, 27.8%), following musculoskeletal disorders (most likely, 33.9%; second most likely, 24.6%) (Fig. 1B).
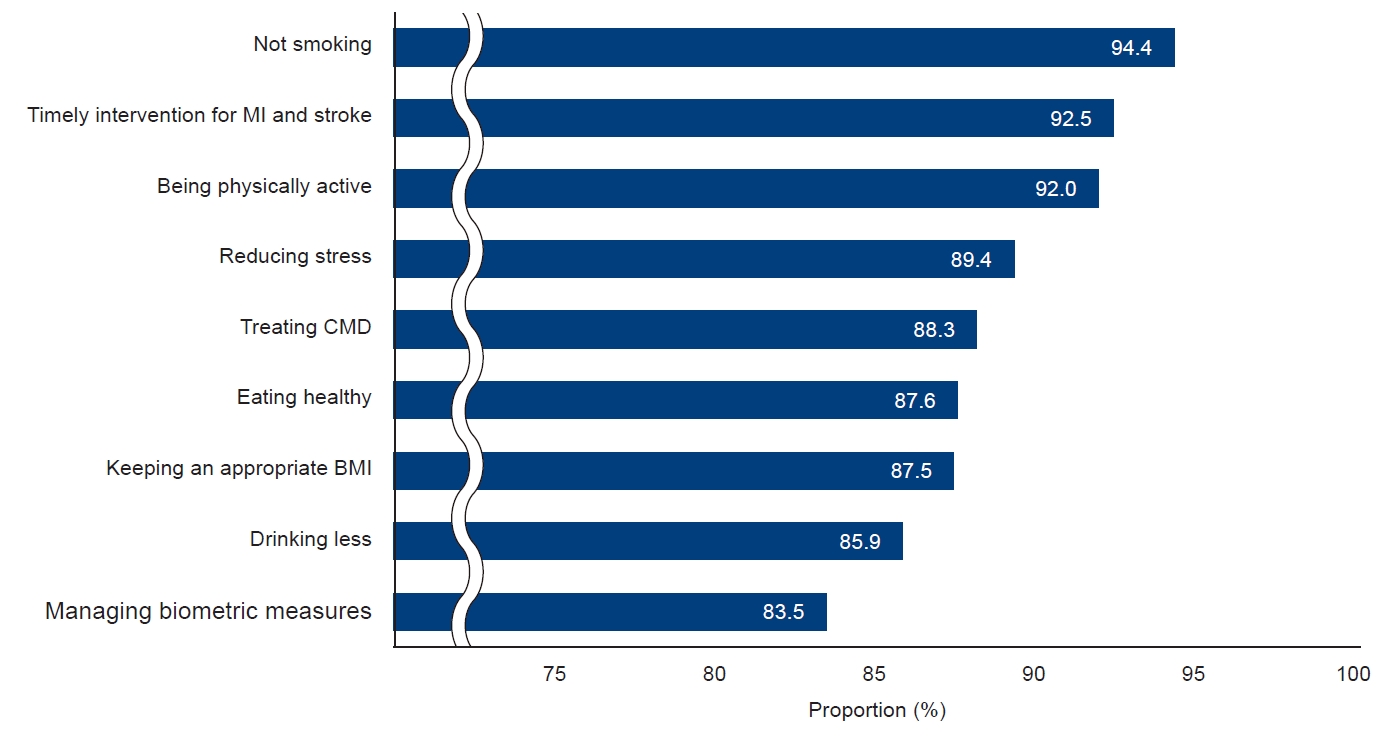
- Among the nine recommendations for CVD prevention, respondents considered "not smoking (94.4%),” "timely intervention for myocardial infarction and stroke (92.5%),” and "being physically active (92.0%)” as the most important. "Managing biometric measures (83.5%)” and "drinking less (85.9%)” were perceived as relatively less important (Fig. 2).
- Respondents ranked “reducing stress (most difficult, 23.2%; second most difficult, 19.9%; third most difficult, 20.1%),” “being physically active (most difficult, 17.4%; second most difficult, 21.4%; third most difficult, 17.6%),” and “eating healthy (most difficult, 18.6%; second most difficult, 17.9%; third most difficult, 18.7%)” as the most challenging lifestyle recommendations (Fig. 3).
- Behavioral changes after the end of social distancing
-
Fig. 4A illustrates the behavioral changes that occurred during the implementation of social distancing measures in response to COVID-19, while Fig. 4B highlights the behavioral changes following the relaxation of these measures. Notably, there was a significant increase in the overall rate of positive behavioral changes after social distancing ended, compared to the period during the pandemic. During COVID-19, stress levels, physical activity, and dietary habits experienced marked negative changes, but these rates substantially decreased following the cessation of social distancing. In particular, the rates of positive changes in physical activity and diet were approximately double those of the negative changes post–social distancing. However, stress levels continued to show a higher rate of negative change (40.0%) compared to positive change (19.5%) even after social distancing measures were lifted. Table S1 presents the adjusted risks of negative changes based on socioeconomic factors. For smoking, the risk of negative change was lower among women and higher among high school graduates. With regard to diet, the risk of negative change decreased with increasing age, and women had a higher risk of negative change than men. For exercise, individuals aged 50 years or older had a lower risk, but women had a higher risk. The likelihood of negative changes in stress was lower in those aged 50 years or older and higher in the bereaved, separated, or divorced group.
-
Table S2 presents the adjusted risks for positive changes based on socioeconomic factors. In the case of smoking, women demonstrated a greater likelihood of positive changes. With respect to alcohol consumption, individuals in their 30s and 40s exhibited a reduced likelihood of positive changes. Concerning diet, those aged 50 years and older, along with women, were more inclined toward positive changes. Women were also more likely to experience positive changes in stress management. Regarding the use of healthcare services, women and individuals with a history of cardiometabolic disease showed a significantly greater likelihood of positive changes.
DISCUSSION
- This study explored public awareness of CVD prevention and the modification of health behaviors following the cessation of social distancing measures. CVD was identified as the second most concerning disease after cancer, and it was perceived as more likely to occur than cancer. Of the nine recommendations for preventing CVD, "reducing stress," "being physically active," and "eating healthy" were deemed the most challenging behaviors to adopt. After social distancing ended, there was a general increase in the reported rates of positive behavioral changes as opposed to negative ones. However, stress levels were an exception, with higher reported rates of negative changes compared to positive ones.
- Previous studies have reported negative changes in several health behaviors during the COVID-19 pandemic [13–15,17]. These negative changes appear to be primarily attributable to social isolation [18,19]. Thus, the overall positive changes observed after the end of social distancing could be considered as a recovery associated with the relaxation of social isolation. However, stress continued to worsen even after the end of social distancing, which could be attributed to changes in the living environment [20]. Further studies are needed to understand the impact of the end of social distancing on stress.
- We investigated sociodemographic factors associated with negative and positive changes after the end of social distancing. For smoking, men and those with a high school education showed higher rates of negative changes and lower rates of positive changes. For alcohol consumption, positive changes were less common in participants in their 30s and 40s. This appears to be a result of the relaxation of restrictions on smoking and drinking environments after the end of social distancing. Regarding diet, younger age groups exhibited higher rates of negative changes. Negative changes in exercise were more prevalent in women, and for stress, the bereaved/separated/divorced group reported higher negative changes, with men showing a lower likelihood of positive changes. Targeted interventions should be directed at groups exhibiting higher negative changes and fewer positive changes in health behaviors following the end of social distancing.
- There are some limitations in this study. First, there is potential recall bias, due to self-reported data without objective measures. Second, the study population may not fully represent the entire Korean population. The survey was conducted online or via mobile devices, which might result in different response rates according to familiarity with electronic devices. Third, the sample size was relatively small, which may have limited the ability to assess associations between behavioral changes and sociodemographic factors. Despite these limitations, a strength of this study is that it specifically investigated changes in health behaviors after the end of social distancing.
- In conclusion, this study revealed a prevailing trend for positive changes in behaviors influencing cardiovascular health after the discontinuation of social distancing, except for stress levels. Further research is essential to fully grasp the implications of ending social distancing on stress, and to explore the long-term effects of social distancing on cardiovascular health.
ARTICLE INFORMATION
-
Conflicts of interest
Hyeon Chang Kim and Won-Young Lee are Consulting Editors of Cardiovascular Prevention and Pharmacotherapy, but were not involved in the peer reviewer selection, evaluation, or decision process of this article. The authors have no other conflicts of interest to declare.
-
Funding
The authors received no financial support for this study.
-
Author contributions
Conceptualization: WYL, EJR, HCK; Data curation: JL, EK, EJR, HCK; Formal analysis: JL; Methodology: EJR, HCK; Project administration: WYL, EJR; Supervision: HCK; Validation: WYL; Visualization: JL, EK; Writing–original draft: JL, HCK; Writing–review & editing: EK, WYL, EJR, HCK. All authors read and approved the final manuscript.
-
Acknowledgments
The current study used data from the 2023 Cardiovascular Disease Prevention Awareness Survey, which was conducted by the Korean Society of Cardiovascular Disease Prevention (KSCP), and surveyed by a professional research agency, Embrain (Seoul, Korea).
Supplementary materials
Table S1. Association between sociodemographic factors and negative changes of cardiovascular-related health behaviors after the end of social distancing
cpp-2024-6-e6-Table-S1.pdf
Table S2. Association between sociodemographic factors and positive changes of cardiovascular-related health behaviors after the end of social distancing
cpp-2024-6-e6-Table-S2.pdf
Supplementary materials are available from https://doi.org/10.36011/cpp.2024.6.e6.
Fig. 1.Among the five diseases surveyed, responses of (A) the most feared disease and (B) the most likely disease to develop within 10 years.
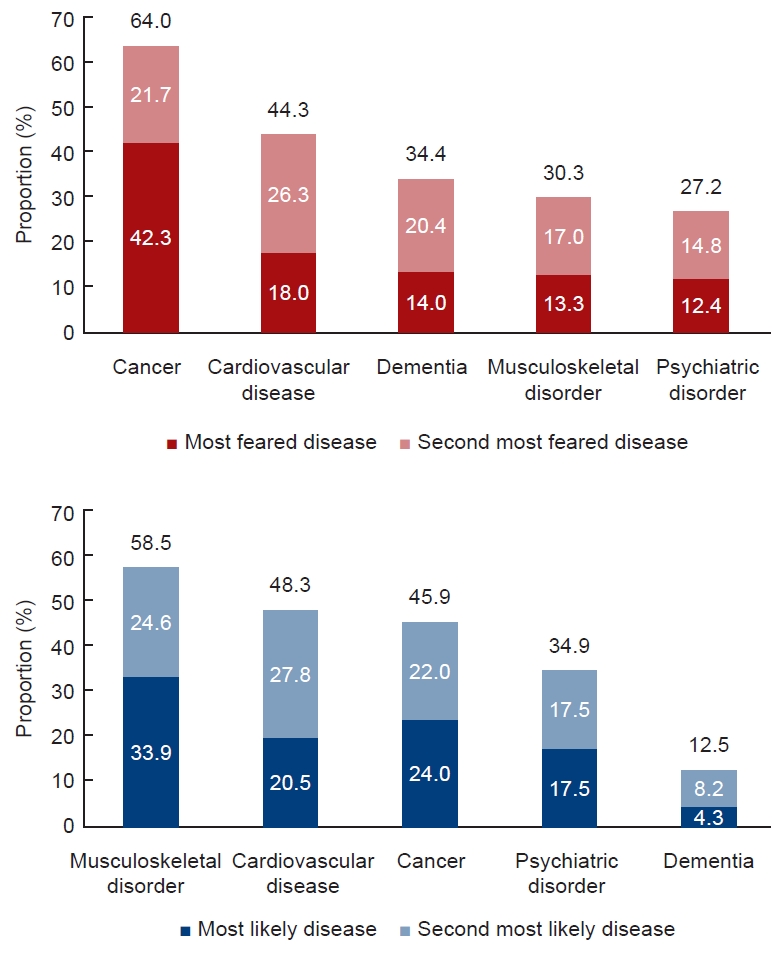
Fig. 2.Perceived importance of each recommendation for cardiovascular disease prevention. MI, myocardial infarction; CMD, cardiometabolic disease; BMI, body mass index.
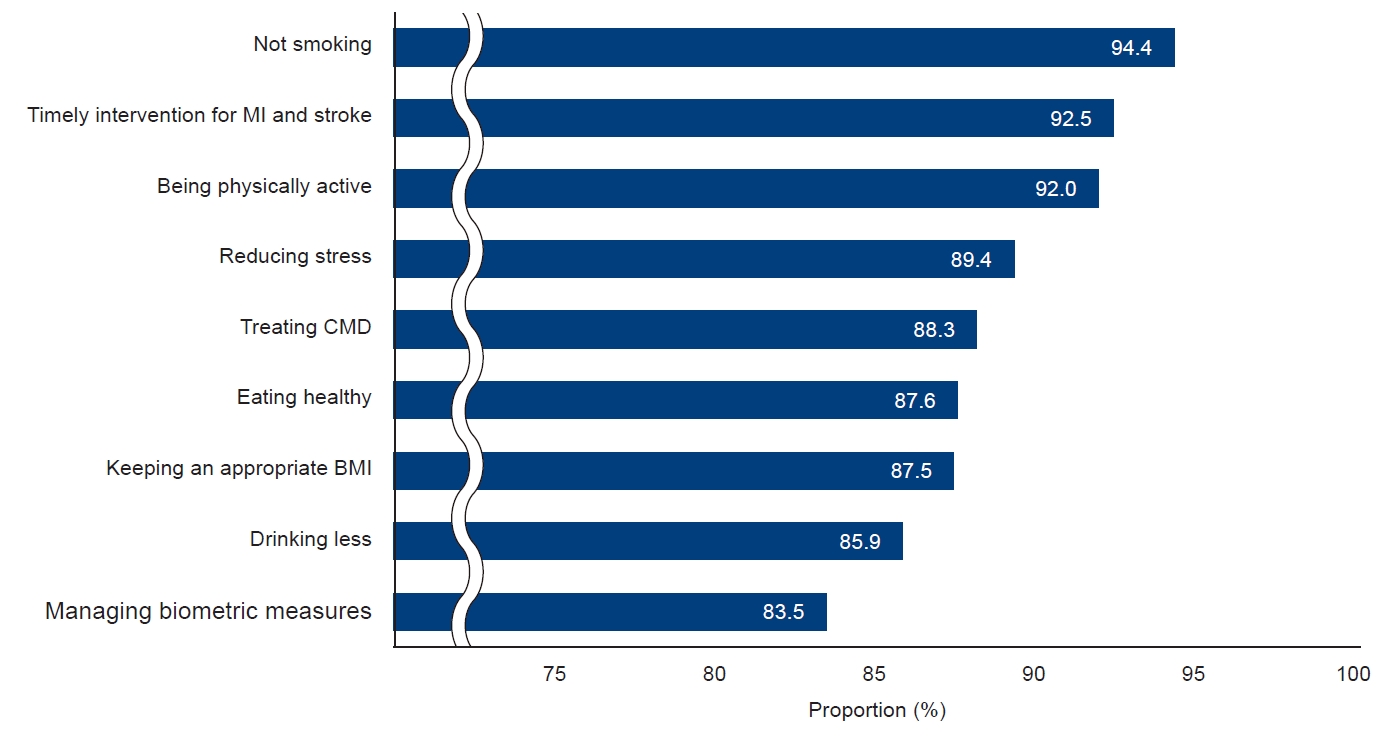
Fig. 3.The most difficult recommendations to follow among nine the recommendations for cardiovascular disease prevention. BMI, body mass index; CMD, cardiometabolic disease; MI, myocardial infarction.

Fig. 4.Changes in cardiovascular-related health behaviors (A) during and (B) after the end of social distancing.

Table 1.General characteristics of the survey participants (n=2,000)
|
Characteristic |
No. of participants (%) |
|
Age (yr) |
|
|
20–29 |
427 (21.4) |
|
30–39 |
446 (22.3) |
|
40–49 |
545 (27.3) |
|
≥50 |
582 (29.1) |
|
Sex |
|
|
Male |
1,027 (51.4) |
|
Female |
973 (48.7) |
|
Marital status |
|
|
Married |
1,080 (54.0) |
|
Single |
824 (41.2) |
|
Bereaved/separated/divorced |
96 (4.8) |
|
Education |
|
|
Middle school or lower |
16 (0.8) |
|
High school |
415 (20.8) |
|
College or higher |
1,569 (78.5) |
|
Monthly household income (KRW) |
|
|
<3 million |
651 (32.6) |
|
3 to <6 million |
901 (45.1) |
|
≥6 million |
448 (22.4) |
|
Cardiometabolic disease |
|
|
None |
1,296 (64.8) |
|
Coronary heart disease |
46 (2.3) |
|
Cerebrovascular disease |
33 (1.7) |
|
Hypertension |
369 (18.5) |
|
Diabetes |
149 (7.5) |
|
Dyslipidemia |
422 (21.1) |
REFERENCES
- 1. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1736–88.ArticlePubMedPMC
- 2. Roth GA, Forouzanfar MH, Moran AE, Barber R, Nguyen G, Feigin VL, et al. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med 2015;372:1333–41.ArticlePubMedPMC
- 3. Zhao D. Epidemiological features of cardiovascular disease in Asia. JACC Asia 2021;1:1–13.ArticlePubMedPMC
- 4. Rodgers JL, Jones J, Bolleddu SI, Vanthenapalli S, Rodgers LE, Shah K, et al. Cardiovascular risks associated with gender and aging. J Cardiovasc Dev Dis 2019;6:19. ArticlePubMedPMC
- 5. Korean Statistical Information Service. Future population projection. Statistics Korea; [updated 2022 May 26; cited 2023 Nov 27]. Available from: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1BPB001&conn_path=I2
- 6. Lloyd-Jones DM, Allen NB, Anderson CA, Black T, Brewer LC, Foraker RE, et al. Life’s essential 8: updating and enhancing the American Heart Association’s Construct of Cardiovascular Health: a presidential advisory from the American Heart Association. Circulation 2022;146:e18–43.ArticlePubMedPMC
- 7. Siervo M, Lara J, Chowdhury S, Ashor A, Oggioni C, Mathers JC. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: a systematic review and meta-analysis. Br J Nutr 2015;113:1–15.ArticlePubMed
- 8. Ahmed HM, Blaha MJ, Nasir K, Rivera JJ, Blumenthal RS. Effects of physical activity on cardiovascular disease. Am J Cardiol 2012;109:288–95.ArticlePubMed
- 9. Hackshaw A, Morris JK, Boniface S, Tang JL, Milenkovic D. Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study reports. BMJ 2018;360:j5855. ArticlePubMedPMC
- 10. Wang D, Li W, Cui X, Meng Y, Zhou M, Xiao L, et al. Sleep duration and risk of coronary heart disease: a systematic review and meta-analysis of prospective cohort studies. Int J Cardiol 2016;219:231–9.ArticlePubMed
- 11. Korea Disease Control and Prevention Agency (KDCA). Chronic disease prevention and management. KDCA; [updated 2023 Aug 30; cited 2023 Nov 27]. Available from: https://www.kdca.go.kr/contents.es?mid=a20303020300
- 12. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open 2020;3:e2019686.ArticlePubMedPMC
- 13. Fuzeki E, Groneberg DA, Banzer W. Physical activity during COVID-19 induced lockdown: recommendations. J Occup Med Toxicol 2020;15:25. ArticlePubMedPMC
- 14. Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 2020;75:2871–2.ArticlePubMedPMC
- 15. Kim E, Jung CH, Kim DJ, Ko SH, Lee HY, Lee KY, et al. Changes in cardiovascular-related health behaviors during the COVID-19 pandemic. Cardiovasc Prev Pharmacother 2023;5:15–23.ArticlePDF
- 16. Yoon J, Yoon SJ. Quantifying burden of disease to measure population health in Korea. J Korean Med Sci 2016;31 Suppl 2(Suppl 2): S101–7.ArticlePubMedPDF
- 17. Lim S, Lim H, Despres JP. Collateral damage of the COVID-19 pandemic on nutritional quality and physical activity: perspective from South Korea. Obesity (Silver Spring) 2020;28:1788–90.ArticlePubMedPMCPDF
- 18. Ferrante G, Camussi E, Piccinelli C, Senore C, Armaroli P, Ortale A, et al. Did social isolation during the SARS-CoV-2 epidemic have an impact on the lifestyles of citizens? Epidemiol Prev 2020;44(5-6 Suppl 2): 353–62.ArticlePubMed
- 19. Pecanha T, Goessler KF, Roschel H, Gualano B. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am J Physiol Heart Circ Physiol 2020;318:H1441–6.ArticlePubMedPMC
- 20. Aldwin C, Stokols D. The effects of environmental change on individuals and groups: some neglected issues in stress research. J Environ Psychol 1988;8:57–75.Article
Citations
Citations to this article as recorded by

 , Eunji Kim1
, Eunji Kim1 , Won-Young Lee2
, Won-Young Lee2 , Eun-Jung Rhee2
, Eun-Jung Rhee2 , Hyeon Chang Kim1
, Hyeon Chang Kim1