ABSTRACT
-
Background
- Remote collaborative care (ReCC) is a legally recognized form of telehealth that facilitates communication between physicians. This study aimed to analyze the effectiveness of ReCC services and establish a foundation for the usefulness and effectiveness of ReCC.
-
Methods
- This retrospective cohort study utilized data from the Digital Healthcare Information System (DHIS) managed by the Korea Social Security Information Service. We extracted data on patients who were registered from January 2017 through September 2023 to investigate the effects of various factors.
-
Results
- A total of 10,407 individuals participated in the remote collaborative consultation service provided by the DHIS. Of these participants, those aged ≥80 years represented 39.2% (4,085 patients), while those aged 70 to 79 years comprised 36.9% (3,838 patients). The conditions treated included hypertension, affecting 69.2% (7,203 patients), and diabetes, affecting 21.1% (2,201 patients). Although various measurement items were recorded, most data beyond blood pressure readings were missing, posing a challenge for analysis. Notably, there was a significant reduction in blood pressure that was sustained at follow-up intervals of 1, 3, 6, and 12 months post-baseline (all P<0.05).
-
Conclusions
- Owing to the lack of data, follow-up assessments for conditions other than hypertension proved to be challenging. Medical staff should increase their focus on and engagement with the system. Remote consultations have demonstrated efficacy in managing hypertension in medically underserved areas, where access to healthcare services is often limited. This suggests the potential for expanded use of remote chronic care in the future.
-
Keywords: Remote collaborative care telehealth; Telemedicine; Hypertension
INTRODUCTION
- As public interest in telemedicine (non–face-to-face medical treatment) pilot projects has increased, so too has the interest in telehealth facilitated by information and communications technology (ICT) [1–3]. Telehealth differs from telemedicine in that it is not limited to patient-doctor interactions; remote collaborative care (ReCC) specifically involves communication among doctors [4,5]. ReCC enables technical support and medical advice to be shared between local medical professionals, who are with the patient, and remote specialists. In Korea, telemedicine is legally permitted only in certain cases, while ReCC is broadly legal, as it is considered a form of professional support within the existing medical law framework [6]. ReCC is particularly valuable in medically underserved areas, such as rural areas, where it helps to mitigate the shortage of resources in local healthcare facilities by providing essential medical technical support [7].
- Recently, there has been a growing recognition of the importance and efficacy of ReCC in medically underserved areas [8]. Furthermore, initiatives have been undertaken to create a range of systems to enhance the effectiveness of ReCC [9,10]. In this study, we analyzed ReCC data collected from a pilot project aimed at providing medical support in medically underserved areas. We evaluated the effectiveness of various ReCC components, laying the groundwork for understanding the future utility and impact of ReCC.
METHODS
- Ethics statement
- This study was approved by the Institutional Review Board of The Catholic University of Korea (No. KC23ZISI0433). Personal identification numbers that could identify patients were removed from the data provided by Korea Social Security Information Service (SSiS). Furthermore, access to the data was restricted to the principal investigator and one co-investigator, who also conducted the statistical analysis directly. The data were stored as an encrypted file on a secure computer. Given the retrospective nature of this study, there was no potential for harm to the patients' mental or physical well-being. The anonymity of the data negated the need for patient consent.
- Digital Healthcare Information System
- The Digital Healthcare Information System (DHIS) is a remote consultation system managed by the SSiS. This platform was established to enhance access to medical care, as well as to manage and prevent diseases among the elderly and chronically ill in medically underserved areas. DHIS facilitates ReCC between medical institutions, enabling medical staff to exchange patient information and offer accurate advice.
- Study population and design
- This retrospective cohort study utilized data extracted from the DHIS. Patient data were retrieved from the DHIS of the SSiS for the period from January 2017 to September 2023, corresponding to the dates of collaboration. The DHIS database included 54 categories of data, which were divided into four main types: patient information (11 categories), measurement information (17 categories), prescription information (11 categories), and questionnaire information (15 categories). The measurement information encompassed a range of clinical parameters, such as systolic blood pressure (SBP) and diastolic blood pressure (DBP), height, weight, body mass index, percent body fat, waist to hip ratio, skeletal muscle mass, body fat mass, fasting and postprandial glucose levels, total cholesterol, and triglycerides. Additional parameters included high- and low-density lipoprotein cholesterol, glycated hemoglobin, and body temperature, among others. The prescription information category contained 11 categories of data, including diagnoses and drug names. The questionnaire category comprised 15 survey items, which covered topics such as diet, smoking habits, and alcohol consumption.
- Based on the index date, we categorized follow-up visits as follows: visits occurring within 1 to 3 months were labeled as “1M,” those within 3 to 6 months as “3M,” visits within 6 to 12 months as “6M,” and any visits after 12 months as “12M.”
- Statistical analysis
- Data are expressed as means±standard deviations for continuous variables, and as numbers with percentages for categorical variables. Pearson chi-square test was used to calculate the P-values for differences according to sex, age, local information, and medical history. All statistical analyses were conducted using SAS ver. 9.4 (SAS Institute). P-values of less than 0.05 were considered to indicate statistical significance.
RESULTS
- Participation in ReCC services
- During the study period, 10,407 individuals participated in ReCC using DHIS (Table 1); of these participants, 68.8% (7,165 patients) were female and 31.2% (3,242 patients) were male. The oldest participant was 122 years old, with an average age of 75.0±10.8 years. Participation rates were highest among those aged ≥80 years (4,085 patients, 39.2%), followed by the 70 to 79 years age group (3,838 patients, 36.9%). Regional participation was most significant in South Chungcheong Province, accounting for 26.9% of the total (2,803 patients). Among the ReCC participants, 69.2% (7,203 patients) had a medical history of hypertension, and 21.1% (2,201 patients) had diabetes mellitus.
- ReCC service follow-up status
- Of the patients who utilized ReCC services, only 69.0% (7,183 patients) had at least one follow-up observation (Table 1). The rate of follow-up visits was significantly higher in women than in men (69.7% vs. 67.4%, P<0.05). Within the groups followed up at least once, 70.6% (2,882 of 4,085 patients) were aged 80 years or older, 70.0% (2,687 of 3,838 patients) were between 70 and 79 years old, and 65.0% (1,614 of 2,484 patients) were younger than 70 years old. There was a significant increase in the follow-up rate with advancing age (P<0.001).
- Follow-up rate by measurement items of ReCC service
- When using ReCC services, the follow-up rate for each measurement item was approximately 77.1% (5,316 of 6,893 patients) for SBP and DBP, around 58% to 59% for blood tests, and about 38% to 45% for physical index measurements (Table 2). However, the remaining items, with the exception of blood pressure, were measured in fewer than 25% of the total patients, which made it challenging to determine the effect of ReCC on these items.
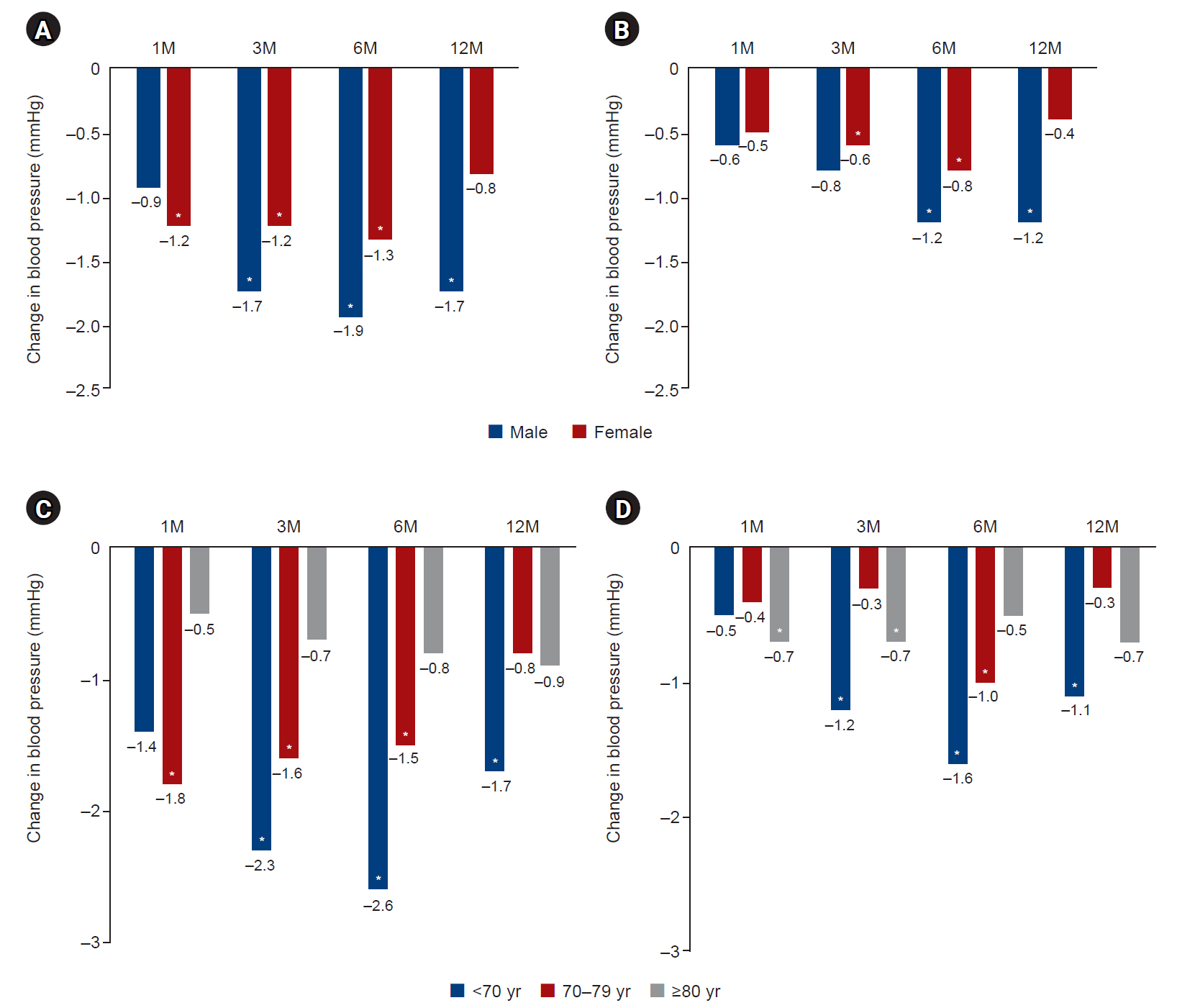
- Tracking changes in blood pressure by sex
- During follow-up, SBP and DBP tended to decrease in both men and women at 1M, 3M, 6M, and 12M follow-up compared to baseline (Fig. 1A, B). Significant reductions were observed in SBP in men at 3M, 6M, and >12M follow-up (–1.7, –1.9, and –1.7 mmHg from baseline, respectively; all P<0.05) and women at 1M, 3M, and 6M follow-up (–1.2, –1.2, and –1.3 mmHg from baseline, respectively; all P<0.05). Significant changes were observed in DBP in men at 6M and 12M (–1.2 and –1.2 mmHg from baseline, respectively; all P<0.05). and in women at 3M and 6M (–0.6 and –0.8 mmHg from baseline, respectively; all P<0.05).
- Blood pressure tracking changes by age
- Over the course of follow-up, SBP and DBP tended to decrease across all ages at 1M, 3M, and 6M follow-up compared to baseline (Fig. 1C, D). Significant changes were observed in SBP for those aged <70 years at follow-up time points of 3M, 6M, and 12M (–2.3, –2.6, and –1.7 mmHg from baseline, respectively; all P<0.05); for those aged 70 to 79 years, the follow-up time points were 1M, 3M, and 6M (–1.8, –1.6, and –1.5 mmHg from baseline, respectively; all P<0.05). Significant changes were observed in DBP for those aged <70 years at the follow-up time points of 3M, 6M, and 12M (–1.2, –1.6, and –1.1 mmHg from baseline, respectively; all P<0.05); for those aged 70 to 79 years at the follow-up time point of 6M (–1.0 mmHg from baseline, P<0.05); and for those aged ≥80 years at the 1M and 3M follow-up points (–0.7 and –0.7 mmHg from baseline, respectively; all P<0.05).
DISCUSSION
- Telehealth is a medical service that utilizes ICT and has recently garnered significant attention alongside telemedicine (non–face-to-face medical treatment) [1–3]. ReCC primarily focuses on medically vulnerable areas [8]. The aim of integrating ICT into healthcare is to effectively distribute high-quality medical resources to areas with limited medical services, enhance both the quality and quantity of medical resources, and deliver efficient medical services. Unlike telemedicine, which involves direct communication between patients and doctors, ReCC encompasses doctor-to-doctor communication. This is expected to facilitate better communication and is anticipated to improve the quality of medical care as well as the efficiency of the healthcare delivery system [11,12].
- In this study, 10,407 patients were enrolled in ReCC between 2017 and 2023. Of these, a significant majority of the remote consultations (76.1%) were with patients aged 70 years or older. ReCC is designed to serve patients in medically underserved areas who face challenges in accessing medical services [8]. Many of these patients are older adults living with chronic conditions. Thus, the predominance of participants over the age of 70 in this study seems to align well with the intended purpose of ReCC. Notably, as of 2020, the prevalence of diabetes among individuals older than 65 years in Korea was 30.1%, and this figure has been on the rise [13]. Specifically, within the female diabetic population, those aged 70 years or older represented the largest segment at 39.7% [13]. Regarding hypertension, studies have shown that prevalence, as well as rates of awareness, treatment, and control, have been increasing among the elderly over time [13,14].
- The ReCC service exhibited the highest participation rates in Chungcheongnam and Jeollanam Provinces. Women represented the majority, comprising two-thirds of the cases. Nonetheless, this trend did not vary significantly across different regions.
- In the current study, hypertension emerged as the most prevalent chronic disease among ReCC participants. The adherence to blood pressure monitoring was notably high, with a significant proportion of patients undergoing the measurement more than twice. This likely reflects the fundamental role of blood pressure assessment in medical practice. It is, however, regrettable that other crucial tests, such as blood and body composition analyses, are not being conducted as consistently. Given the recurrent nature of chronic diseases, the frequent prescription of medication was an expected finding. Nevertheless, in light of ReCC's objective to facilitate patient health management through the use of ICT [7], the lack of comprehensive testing is a concern. This issue warrants attention and should be addressed in future research.
- Most clinical studies on hypertension have demonstrated that reducing SBP by 10 to 20 mmHg and DBP by 5 to 10 mmHg can decrease the risk of stroke by 30% to 40% and the risk of ischemic heart disease by 15% to 20% [15,16]. In this study, however, the use of the ReCC service significantly improved both SBP and DBP across all age groups. Considering the role of ReCC in medically underserved areas where access to medical services is limited [8], these findings indicate that hypertension, as a chronic condition, may be effectively managed through remote consultation. Regrettably, due to a lack of data, this study was only able to evaluate hypertension outcomes after follow-up. Nonetheless, we are optimistic that these results will lay the groundwork for extending such services to other chronic diseases in the future.
- Arthritis, diabetes mellitus, and hyperlipidemia are prevalent comorbidities and represent the most common chronic diseases among the elderly [17–19]. This study offers guidance on which diseases would benefit from future research on ReCC. Telehealth, facilitated by ICT, has been shown to be more effective for managing chronic diseases than acute conditions [20], and its various possibilities and effects have been proven scientifically [21,22].
- In medically underserved areas, local clinics may not have the same level of medical expertise as larger hospitals in metropolitan regions. Strengthening the connections between remote medical institutions and local clinics can significantly enhance healthcare delivery. To maximize this benefit, it is essential to implement a system that facilitates the immediate transmission and exchange of data and opinions to assess a patient's health status [1]. An effective ReCC system is necessary to provide treatment without requiring patients to visit a remote medical institution in person. This requires a platform that supports communication between local clinics and remote medical institutions [1]. Additionally, medical staff should have the capability to make voice and video calls, share screens, and exchange documents. Before such a platform can be commercialized, issues of reliability and security must be addressed [23,24]. Although the current SSiS DHIS was expected to perform effectively, it has not lived up to expectations. This shortfall seems to stem from low active engagement by medical staff rather than from system deficiencies. It is important to focus on the medical personnel at these institutions who are utilizing the technology. Since the ReCC's objective is to facilitate diagnoses and prescriptions, the active involvement of remote doctors is essential.
- This study had several limitations because of its retrospective cohort design [25,26]. First, considerable data were missing. The missing data made it difficult to further analyze various diseases, including diabetes. The lack of active utilization by medical staff was apparent, and it is critical to explore methods to foster their active engagement. Consequently, the fee structure for ReCC warrants discussion. ReCC encompasses a range of modalities, such as teleconsultation and video consultation; however, our research was limited to remote collaboration in medically underserved areas. The inability to examine the topic from multiple angles was another limitation of this study.
- Some doctors are unaware that ReCC is legal [6], unlike non–face-to-face medical treatment. Consequently, there is a need for proactive national promotion. Hypertension is the most significant risk factor for cardiovascular diseases among the elderly. With the accumulation of experience from repeated ReCC sessions, a standardized treatment approach can be developed. There is an immediate need for guidelines and recommendations to govern the use of ReCC. Therefore, to ascertain whether long-term management of blood pressure via ReCC in the elderly can contribute to cardiovascular disease risk management, further research is necessary.
ARTICLE INFORMATION
-
Author contributions
Conceptualization: SYB, HSK; Data curation: all authors; Formal analysis: SYB, KMK, HSK; Funding acquisition: HSK; Investigation: HSK; Methodology: HSK; Project administration: HSK; Resources: HSK; Software: HSK; Supervision: HSK; Validation: HSK; Visualization: SYB; Writing–original draft: SYB; Writing–review & editing: all authors. All authors read and approved the final manuscript.
-
Conflicts of interest
The authors have no conflicts of interest to declare.
-
Funding
This study was supported by a grant for the Teleconsultation in Medically Underserved Areas (MUAs), funded by the Korean Ministry of Health and Welfare.
Fig. 1.Changes in blood pressure by (A, B) sex and (C, D) age. (A, C) Systolic blood pressure. (B, D) Diastolic blood pressure. Visits occurring within 1 to 3 months were labeled as “1M,” those within 3 to 6 months as “3M,” visits within 6 to 12 months as “6M,” and any visits after 12 months as “12M.” *P<0.05 (paired t-test from baseline).
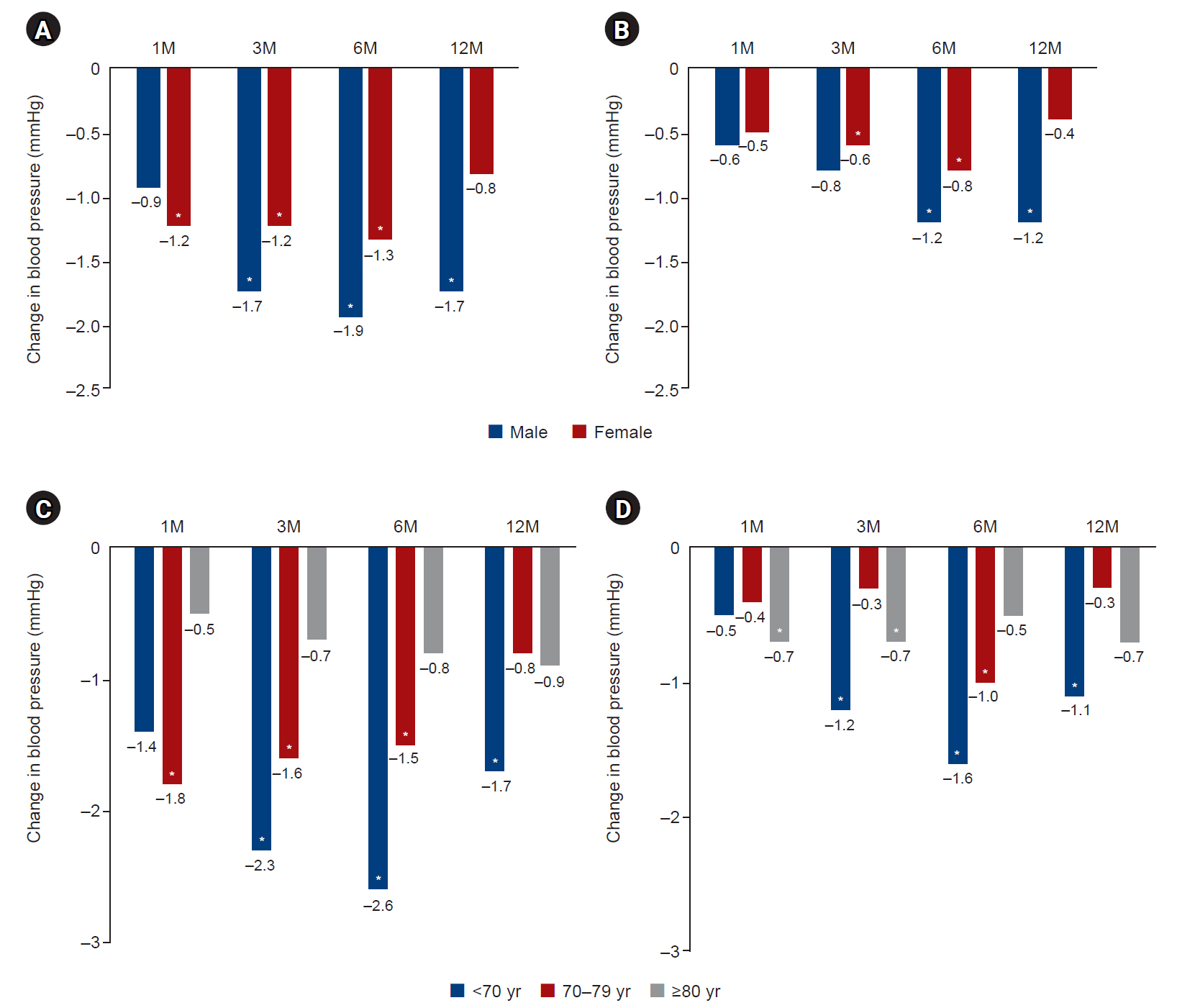
Table 1.Participation level in remote collaborative care services
|
Variable |
Total |
Follow-up |
P-valuea)
|
|
No. of patients |
10,407 (100) |
7,183 (69.0) |
|
|
Sex |
|
|
<0.05 |
|
Male |
3,242 (31.2) |
2,186 (67.4) |
|
|
Female |
7,165 (68.8) |
4,997 (69.7) |
|
|
Age (yr) |
75.0±10.8 |
- |
<0.001 |
|
<70 |
2,484 (23.9) |
1,614 (65.0) |
|
|
70–79 |
3,838 (36.9) |
2,687 (70.0) |
|
|
≥80 |
4,085 (39.2) |
2,882 (70.6) |
|
|
Province |
|
|
<0.001 |
|
South Chungcheong |
2,803 (26.9) |
2,212 (78.9) |
|
|
South Jeolla |
2,726 (26.2) |
1,462 (53.6) |
|
|
South Gyeongsang |
1,710 (16.4) |
1,094 (64.0) |
|
|
Gangwon |
1,414 (13.6) |
931 (65.8) |
|
|
North Gyeongsang |
1,052 (10.1) |
900 (85.6) |
|
|
Incheon |
402 (3.9) |
327 (81.3) |
|
|
North Jeolla |
243 (2.3) |
215 (88.5) |
|
|
Jeju |
51 (0.5) |
37 (72.5) |
|
|
Gyeonggi |
6 (0.1) |
5 (83.3) |
|
|
Current illness |
|
|
<0.001 |
|
Hypertension |
7,203 (69.2) |
5,444 (75.6) |
|
|
Diabetes mellitus |
2,201 (21.1) |
1,593 (72.4) |
|
|
Arthritis |
2,148 (20.6) |
1,360 (63.3) |
|
|
Dyslipidemia |
1,788 (17.2) |
1,439 (80.5) |
|
|
Other |
3,365 (32.3) |
2,034 (60.4) |
|
Table 2.Follow-up rate by measurement item in remote collaborative medical service
|
Variable |
No. of patients |
Follow-up rate (%) |
|
Measured at least once |
Follow-up |
|
Systolic hypertension (mmHg) |
6,893 |
5,316 |
77.1 |
|
Diastolic hypertension (mmHg) |
6,893 |
5,316 |
77.1 |
|
Pulse rate (beats/min) |
5,781 |
4,488 |
77.6 |
|
Total cholesterol (mmol/L) |
2,262 |
1,272 |
56.2 |
|
Triglyceride (mmol/L) |
1,456 |
855 |
58.7 |
|
High-density lipoprotein cholesterol (mmol/L) |
1,393 |
823 |
59.1 |
|
Low-density lipoprotein cholesterol (mmol/L) |
1,356 |
802 |
59.1 |
|
Fasting glucose (mmol/L) |
1,327 |
512 |
38.6 |
|
Weight (kg) |
1,202 |
466 |
38.8 |
|
Height (cm) |
1,183 |
444 |
37.5 |
|
Body mass index (kg/m2) |
1,108 |
424 |
38.3 |
|
Glycated hemoglobin (mmol/L) |
1,011 |
587 |
58.1 |
|
Percent body fat (%) |
549 |
224 |
40.8 |
|
Body fat mass (kg) |
523 |
231 |
44.2 |
|
Waist to hip ratio |
515 |
222 |
43.1 |
|
Skeletal muscle mass (kg) |
507 |
226 |
44.6 |
REFERENCES
- 1. Park JI, Lee HY, Kim H, Lee J, Shinn J, Kim HS. Lack of acceptance of digital healthcare in the medical market: addressing old problems raised by various clinical professionals and developing possible solutions. J Korean Med Sci 2021;36:e253.ArticlePubMedPMCPDF
- 2. Kim HS. Apprehensions about excessive belief in digital therapeutics: points of concern excluding merits. J Korean Med Sci 2020;35:e373.ArticlePubMedPMCPDF
- 3. Kim HS, Yoon KH. Lessons from use of continuous glucose monitoring systems in digital healthcare. Endocrinol Metab (Seoul) 2020;35:541–8.ArticlePubMedPMCPDF
- 4. Swar S, Rimal P, Gauchan B, Maru D, Yang Y, Acharya B. Delivering collaborative care in rural settings: integrating remote teleconsultation and local supervision in rural Nepal. Psychiatr Serv 2019;70:78–81.ArticlePubMedPMC
- 5. Hayashi Y, Yokoyama Y, Kazama T, Hirayama D, Nakase H. Report on a new remote collaborative medical care system -construction and operation of a remote collaborative medical care network for inflammatory bowel disease using information and communication technology in Hokkaido. Nihon Shokakibyo Gakkai Zasshi 2022;119:830–8.ArticlePubMed
- 6. Korea Law Translation Center. Medical Service Act. Act No. 18468 (September 24, 2021), Article 34, Paragraph (1). Korea Legislation Research Institute; 2023 [cited 2023 Sep 1]. Available from: https://elaw.klri.re.kr/eng_service/lawView.do?hseq=64153&lang=ENG
- 7. Gasvaer JI, Jepsen R, Heldal I, Sudmann T. Supporting collaboration in rehabilitation trajectories with information and communication technologies: scoping review. JMIR Rehabil Assist Technol 2023;10:e46408.ArticlePubMedPMC
- 8. Clavagnier I. Telemedicine, remote collaboration. Rev Infirm 2017;66:24–6.Article
- 9. Zhou Y, Luo B, Sang J, Li C, Zhu M, Zhu Z, et al. A cloud-based consultation and collaboration system for radiotherapy: remote decision support services for community radiotherapy centers. Comput Methods Programs Biomed 2023;229:107270. ArticlePubMed
- 10. Branzan Albu A, Laurendeau D, Gurtner M, Martel C. A web-based remote collaborative system for visualization and assessment of semi-automatic diagnosis of liver cancer from CT images. Stud Health Technol Inform 2005;111:75–8.PubMed
- 11. Lv H, Yang G, Zhou H, Huang X, Yang H, Pang Z. Teleoperation of collaborative robot for remote dementia care in home environments. IEEE J Transl Eng Health Med 2020;8:1400510. ArticlePubMedPMC
- 12. Rojas G, Guajardo V, Martínez P, Castro A, Fritsch R, Moessner M, et al. A remote collaborative care program for patients with depression living in rural areas: open-label trial. J Med Internet Res 2018;20:e158.ArticlePubMedPMC
- 13. Bae JH, Han KD, Ko SH, Yang YS, Choi JH, Choi KM, et al. Diabetes fact sheet in Korea 2021. Diabetes Metab J 2022;46:417–26.ArticlePubMedPMCPDF
- 14. Yan Y, Wu T, Zhang M, Li C, Liu Q, Li F. Prevalence, awareness and control of type 2 diabetes mellitus and risk factors in Chinese elderly population. BMC Public Health 2022;22:1382. ArticlePubMedPMCPDF
- 15. Kim HC, Lee H, Lee HH, Lee G, Kim E, Song M, et al. Korea hypertension fact sheet 2022: analysis of nationwide population-based data with a special focus on hypertension in the elderly. Clin Hypertens 2023;29:22. ArticlePubMedPMCPDF
- 16. Lewington S, Clarke R, Qizilbash N, Peto R, Collins R; Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360:1903–13.ArticlePubMed
- 17. Uchiyama S, Takanashi S, Takeno M, Gono T, Kaneko Y, Takeuchi T, et al. Should we reconsider the definition of elderly-onset rheumatoid arthritis in an ageing society? Mod Rheumatol 2022;32:323–9.ArticlePubMedPDF
- 18. Zeyfang A, Wernecke J, Bahrmann A. Diabetes mellitus at an elderly age. Exp Clin Endocrinol Diabetes 2021;129(S 01):S20–6.Article
- 19. Lucchi T. Dyslipidemia and prevention of atherosclerotic cardiovascular disease in the elderly. Minerva Med 2021;112:804–16.ArticlePubMed
- 20. Kim HS, Hwang Y, Lee JH, Oh HY, Kim YJ, Kwon HY, et al. Future prospects of health management systems using cellular phones. Telemed J E Health 2014;20:544–51.ArticlePubMedPMC
- 21. Shigekawa E, Fix M, Corbett G, Roby DH, Coffman J. The current state of telehealth evidence: a rapid review. Health Aff (Millwood) 2018;37:1975–82.ArticlePubMed
- 22. Kim HS, Kim H, Lee S, Lee KH, Kim JH. Current clinical status of telehealth in Korea: categories, scientific basis, and obstacles. Healthc Inform Res 2015;21:244–50.ArticlePubMedPMC
- 23. Camarines TM, Camarines JC. Discussing data security and telehealth during the COVID-19 pandemic. J Public Health (Oxf) 2022;44:e449–50.ArticlePubMedPMCPDF
- 24. Ahmad RW, Salah K, Jayaraman R, Yaqoob I, Ellahham S, Omar M. The role of blockchain technology in telehealth and telemedicine. Int J Med Inform 2021;148:104399. ArticlePubMedPMC
- 25. Kim HS, Kim JH. Proceed with caution when using real world data and real world evidence. J Korean Med Sci 2019;34:e28.ArticlePubMedPMCPDF
- 26. Kim HS, Kim DJ, Yoon KH. Medical big data is not yet available: why we need realism rather than exaggeration. Endocrinol Metab (Seoul) 2019;34:349–54.ArticlePubMedPMCPDF
Citations
Citations to this article as recorded by

 , Kyoung Min Kim2
, Kyoung Min Kim2 , Hakyoung Park3
, Hakyoung Park3 , Jiwon Shinn3
, Jiwon Shinn3 , Hun-Sung Kim3,4
, Hun-Sung Kim3,4