 , Maria Patricia Inggriani1
, Maria Patricia Inggriani1 , Brilliant Winona Jhundy1
, Brilliant Winona Jhundy1 , Jajah Fachiroh2,3
, Jajah Fachiroh2,3 , Putri Tiara Rosha3,4
, Putri Tiara Rosha3,4 , Ratri Kusuma Wardani3,5
, Ratri Kusuma Wardani3,5 , Fatwa Sari Tetra Dewi3,5
, Fatwa Sari Tetra Dewi3,5
1Department of Cardiology and Vascular Medicine, Dr. Sardjito Hospital, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia
2Department of Histology and Cell Biology, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia
3Health and Demographic Surveillance System (HDSS) Sleman, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia
4Department of Public Health Science, Faculty of Sport Science, Universitas Negeri Semarang, Semarang, Indonesia
5Department of Health Behavior, Environment and Social Medicine, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Yogyakarta, Indonesia
Copyright © 2023 Korean Society of Cardiovascular Disease Prevention; Korean Society of Cardiovascular Pharmacotherapy.
This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Ethical statements
This study protocol was approved by the Medical and Health Research Ethics Committee of Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada (UGM) and Dr Sardjito Hospital (No. KE/FK/0434/EC/2018 and No. KE/FK/0526/EC/2019). All subjects provided written informed consent to participate in the Health and Demographic Surveillance System (HDSS) Sleman survey, which included consent for the use of the data from the UGM HDSS Sleman database for research purposes.
Conflicts of interest
The authors have no conflicts of interest to declare.
Funding
This study was funded by the Indonesia Ministry of Education, Culture, Research, and Technology through UGM under the scheme of “Penelitian Dasar Unggulan Perguruan Tinggi (Basic Research Excellence in Higher Education)” (No. 1657/UN1/DITLIT/DIT-LIT/PT/2021 and No. 6499/UN1/DITLIT/DIT-LIT/PT/2021) with Anggoro Budi Hartopo as the principal investigator.
Acknowledgments
The authors are thankful to the staff of the HDSS Sleman, Faculty of Medicine, Public Health, and Nursing, UGM for their invaluable assistance with data collection and subject selection. The authors are also grateful to Dr. Adysti Dhian Rizky Paramytha and Dr. Aras Amilla Husna for their role as research assistants in collecting data on stable coronary artery disease subjects. The authors also acknowledge the Language Clinic at the Faculty of Medicine, Public Health, and Nursing, UGM for their help in editing and correcting the English language in this manuscript.
Author contributions
Conceptualization: ABH, JF, FSTD; Data curation: ABH, MPI, BWJ, PTR, RKW, FSTD; Formal Analysis: ABH, MPI, BWJ, JF, PTR; Funding acquisition: ABH; Investigation: MPI, RKW; Methodology: all authors; Project administration: FSTD; Resources: FSTD; Software: PTR, RKW; Supervision: ABH, JF, FSTD; Validation: ABH, JF, FSTD; Visualization: ABH, PTR; Writing–original draft: ABH, MPI, BWJ, PTR, RKW; Writing–review & editing: ABH, JF, FSTD. All authors read and approved the final manuscript.
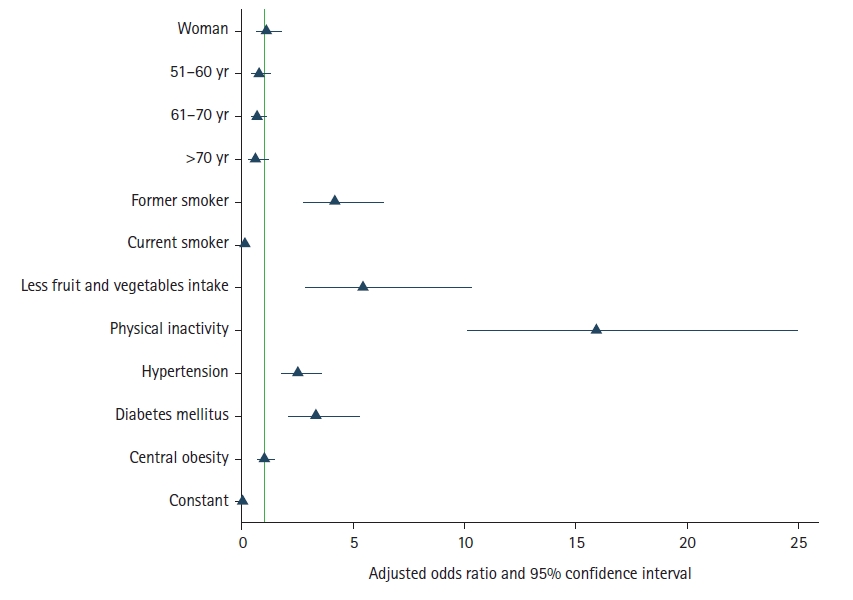
Model 1, ORs adjusted for demographic characteristics (sex and age) and lifestyle-related risk factors (smoking, physical inactivity, and less fruit and vegetable intake). Model 2, ORs adjusted for demographic characteristics (sex and age), clinical risk factors (hypertension, diabetes mellitus, and central obesity) and lifestyle-related risk factors (smoking, physical inactivity, and less fruit and vegetable intake).
OR, odds ratio; NA, not applicable; WHO, World Health Organization; MET, metabolic equivalent of task.
